Reflecting on our COVID experience to improve care by Paul Gimson, Programme Lead, Improvement Cymru
COVID has been a traumatic experience for many who work in the NHS. Battlefield scenes, redeployment and it can seem there is little end in sight. However, there have been positives. Improved team work, new ways of delivering care and better use of technology.
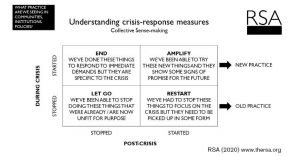
How can we use this learning? How can we ensure that we capture the good stuff, and make sure that we don’t go back to old habits? An article by the Royal Society of the Arts How to create real, lasting change after Covid-19 perhaps offers us some help. It talks about 4 different types of activity that have happened during COVID and how we might respond to them;
- Obsolete Activity; These things were already not fit for purpose but before the crisis we carried on doing them anyway. Our response to COVID has given us the opportunity to stop doing these forever.
- Paused Activity; These are the things we stopped doing to make room for COVID but we will have to restart them at some point.
- Temporary Measures; These are the things we have had to do I response to the immediate demands but they are specific to the crisis and at some point we need to stop doing them
- Innovative Measures; These are the new things we have been able to try. We need to now amplify these and spread the learning across the service.
Based on this we have developed a ‘Learning from COVID’ toolkit’. It is based on the idea that bringing teams together to consider these questions in a facilitated discussion is not only practically helpful in supporting the service to develop – it is important in helping those individuals involved reflect on and come to terms with what they have experiences.
The toolkit explores the three phases of how we normally respond to a crisis;
- Emergency – at the beginning of a crisis there is high energy. A sense of urgency and a common goal brings teams together and things get done.
- Regression – our sense of purpose becomes less clear, energy levels drop, people get frustrated and are less productive.
- Recovery – new goals emerge, and we begin to focus on rebuilding rather than simply surviving. An end, or at least a new sense of normality, is in sight.
How are you feeling now? You could argue that most in the NHS at the moment are in the Regression phase. The aim of this framework is to help people begin to think about how they might move to Recovery.
The workshop consists of a 90 minute session that can be delivered online or in person. It is by no means a quick fix and is only the beginning – it should be done as part of a longer commitment to move toward the recovery phase. It can be emotional. Asking people to reflect on their COVID experience can bring out many feelings. Only experienced facilitators should attempt to deliver it, and anyone who does attempt it must make sure they are ready to support the wellbeing of their team.
But it is worth it. Those we have run the workshop with have found the opportunity to reflect on their COVID experience a positive one. It has helped them to begin to move on. There have been tears but there has also been a sense of excitement about the possibilities that are emerging from it.
The toolkit, along with some guidance on how to run it, are available here;
For more information or support on using the toolkit please contact paul.gimson@wales.nhs.uk