Building an Intermediate Care Team by NHS Wales Awards 2022 winners – Hywel Dda University Health Board
As we approach a year since our fantastic team won two NHS Wales awards, we are fortunate enough to be able to reflect on the success and journey since. As a team we are wedded to the status quo of improving the lives of our ageing population. We aim to prevent deconditioning where possible, to ensure all patients have the opportunity and support, to live independent and fulfilled lives. Our mission is to respond to patients with the right help, in the right place, at the right time, with what’s important to them at the forefront of our decision making.
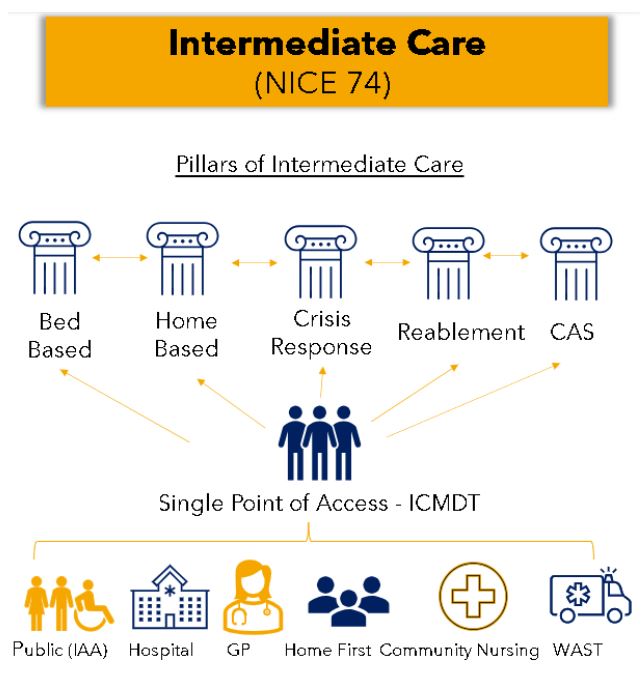
Delivering ‘Home First’ was a strategy set out by the Welsh Government in May (2021), to deliver a component of the ‘A Healthier Wales: Our Plan for Health and Social Care” policy in (2018) which outlines a shift from the reliance on traditional hospital services to a seamless approach of integrated care between health, social and third sector services to deliver care closer to home. Cultivating the mindset of “Home today, if not, why not, and when” which can be applied with the person in their home and in hospital.
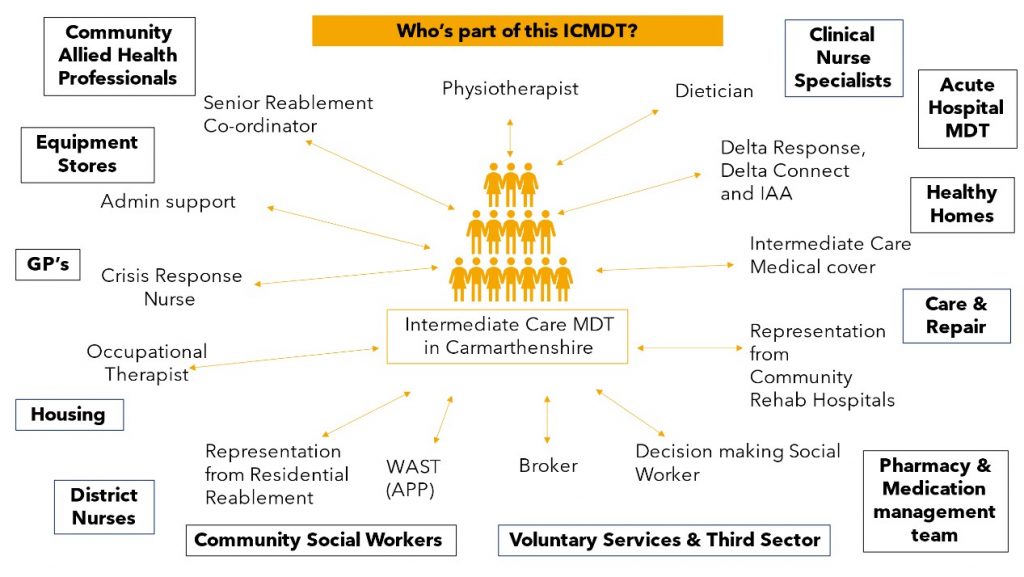
Here in Carmarthenshire, the Home First team encompasses our GP’s, District and Specialist Nurses, Community Allied Health Professionals (AHP’s), Social Workers, Delta Connect, Third Sector and Voluntary Services, Intermediate Care Services, Domiciliary Care Services, Residential and Nursing homes. All working together, prioritising proactive and preventative approaches through to crisis response approaches to optimise healthier days at home for the population, avoid unnecessary hospital admissions and facilitate their discharges home from hospital as soon as possible. This Intermediate Care Services, streamlined through a single point of access that is the Intermediate Care Multi-Disciplinary Team (ICMDT), and its significance in delivering ‘Home First’ in Carmarthenshire was initially introduced in October 2021.
The fundamental principle of the ICMDT is to:
- Facilitate discharge from hospital: All patients are discharged from hospital as soon as medically optimised for a period of assessment and rehab at home, or in one of our bed-based facilities.
- Prevent admission to hospital: All patients who are medically suitable for treatment in the community are supported in their own home by the multidisciplinary response of ICMDT. These referrals often come from the Welsh Ambulance Service, and we are now accepting referrals from more community services, as we approach phase 2.
Winning at the NHS Wales Awards 2022
At the time we entered the awards, we were at the very beginning of our journey. However, there had already been so much development and growth in a short space of time, we were confident as a team to showcase our achievements and what we had learned.
We knew our approach and achievements in this short time were unique so we were hopeful that our efforts wouldn’t go unnoticed. We were delighted to win two awards: ‘Delivering person-centred services’ and ‘Outstanding contribution to transforming health and care’.
It came at a time when we were facing the most unprecedented pressures the health and care system have ever experienced. We had to adapt to change in times of crisis. The achievements of the team demonstrates that even during these times they continue to strive to provide a responsive, caring and effective service to our patients and service users and collaborate with other professionals in times of uncertainty and change.
We want the wider networks to recognise the benefits of an integrated / multi agency nature of the ICMDT which now of course includes our Welsh Ambulance Services Trust (WAST) colleagues. Without the dynamic, passionate workforce this mission would not be possible.
What happened next?
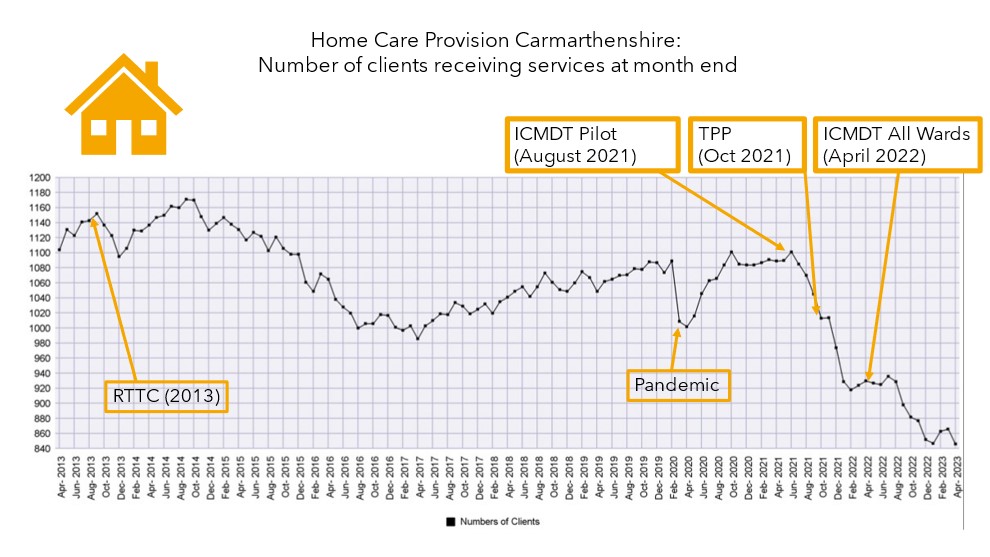
As the graph above demonstrates through the work of ICMDT, the number of people needing long-term social prescriptions has halved. Through utilising professionals such as physiotherapists, occupational therapists, dieticians, therapy support workers (TAPs), nursing teams, GP’s, physician associates, advanced nurse practitioners, admin co-ordinators, advanced paramedic practitioners and social workers, we really do have a co-locating multidisciplinary team work ethic. This enables seamless triage, referrals, discussions and plans to take place.
In the last 9 months the team has dramatically expanded. We have 11 new therapy support workers who work alongside the occupational therapist and physiotherapy team to rehab patients in their own homes. They encourage independence, support with tasks with a ‘hands’ off approach to allow patients to develop the skills for independent living. If needed, they then support patients with third sector referrals such as delta connect. They are an invaluable asset to our ICMDT.
Challenges
We must start by acknowledging our ageing population – a 3% increase in demographic growth per year. Therefore, we must work together smarter, not harder to advocate for the needs of our population (Further, Faster 2023).
There is always room for improved communication, collaboration and integration between health and social care. We are promoting this through co-locating, triaging, and working closely together which encourages equal partnership between health and social care. This will hopefully avoid duplication of work and resources going forward.
Integration between primary care and intermediate care has yet to be established due to capacity and ability as we have been growing the team. However, we hope this will come with phase 2. This will allow us to achieve one of our goals of early prevention and intervention in patients’ homes.
We must also recognise that the length of stay for patients over the age of 65 is 21 days or more in the acute setting. We have been aiming to discharge patients with our support as soon as they are medically optimised, however, we still have some work to do. We aim to deliver an intermediate care service within 72 hours from receipt of referral which we do often achieve, however, there are times we are not managing this due to capacity. We hope to overcome this by further building community capacity and the work force.
Achievements
Our bed-based settings have now been changed under a ‘reablement’ management which have improved the outcomes of patients needing long term care. Our statistics show that the average length of stay is now 30 days and 87% of patients who are discharged do not require any service to go home.
Our advanced paramedic practitioners (APP) pilot has been running for a year. By triaging all 999 calls we have managed to find suitable alternative community pathways in more than 60% of cases thereby saving a 999 conveyance and potential hospital admission.
Between June 2022 – May 2023, 2002 patients were triaged, of which only 39% attended A&E (33% by ambulance and 6% by own transport or through use of third sector resources such as Delta). 4% to alternative areas such as the same day emergency care unit. 8% of those cases were referred to ICMDT for a multi-disciplinary team (MDT) response in a crisis. 21% were treated at scene through the guidance of very experiences advanced clinicians. 20% back to own GP or out of hours GP. 1% referred to district nurses.
When ICMDT alongside advanced paramedic practitioner (APP) are not operational, the stats are flipped back to 60% conveyance to A&E.
We feel the statistics highlight the importance of multidisciplinary co-locating teamwork. We have access to a range of IT systems such as primary care, social care, WAST and secondary care documentation. Together we foster a culture of positive risk taking, building therapeutic relationships with other professionals through education, training, and empowerment.
As a team, our biggest highlight is always positive patient feedback and success stories. Since recruiting our very experienced lead dietician Rachel Budge, we have seen fantastic patient outcomes when good nutrition, rehab and holistic care are used together. One of our recent patients said: “The team used to come in and make my meals, but now I do all my meals myself and the supplements I’m sure, has helped my weight increase which is good news”.
Next: Expansion of the team and further integration with community services
In this next year, we plan to further integrate into secondary care and fully move into phase 2. This will allow us to take direct community referrals into ICMDT.

Our two lead specialist physiotherapists, Leanne Walters and Adele Davies recently attended ‘The Right to Rehab: State of the Nation’ to deliver a talk on ICMDT in the community. Their presentation highlighted to all who attended the benefits of early physiotherapy and reablement on patient outcomes.
We aim to continue to educate, expand and support our ageing population and NHS services to the best of our ability.
For more info, contact Leah Williams, IC MDT Project Manager leah.williams4@wales.nhs.uk.
Take a look at the finalists for this year’s NHS Wales Awards at nhsawards.wales.